Did you know chronic nasal obstruction and/or open mouth breathing during early childhood influences the way the face grows?
The impact depends on the extent and duration of facial muscle adaptations.
One of the most recognized patterns of facial growth linked to mouth breathing is a vertical growth pattern called “Adenoid facies” or “long face syndrome.”
Signs to look out for include
- Long and narrow face
- Recessed chin
- Dark circles under the eyes
- Inability to seal lips together without strain
- Narrow v-shaped palate
- Crooked teeth
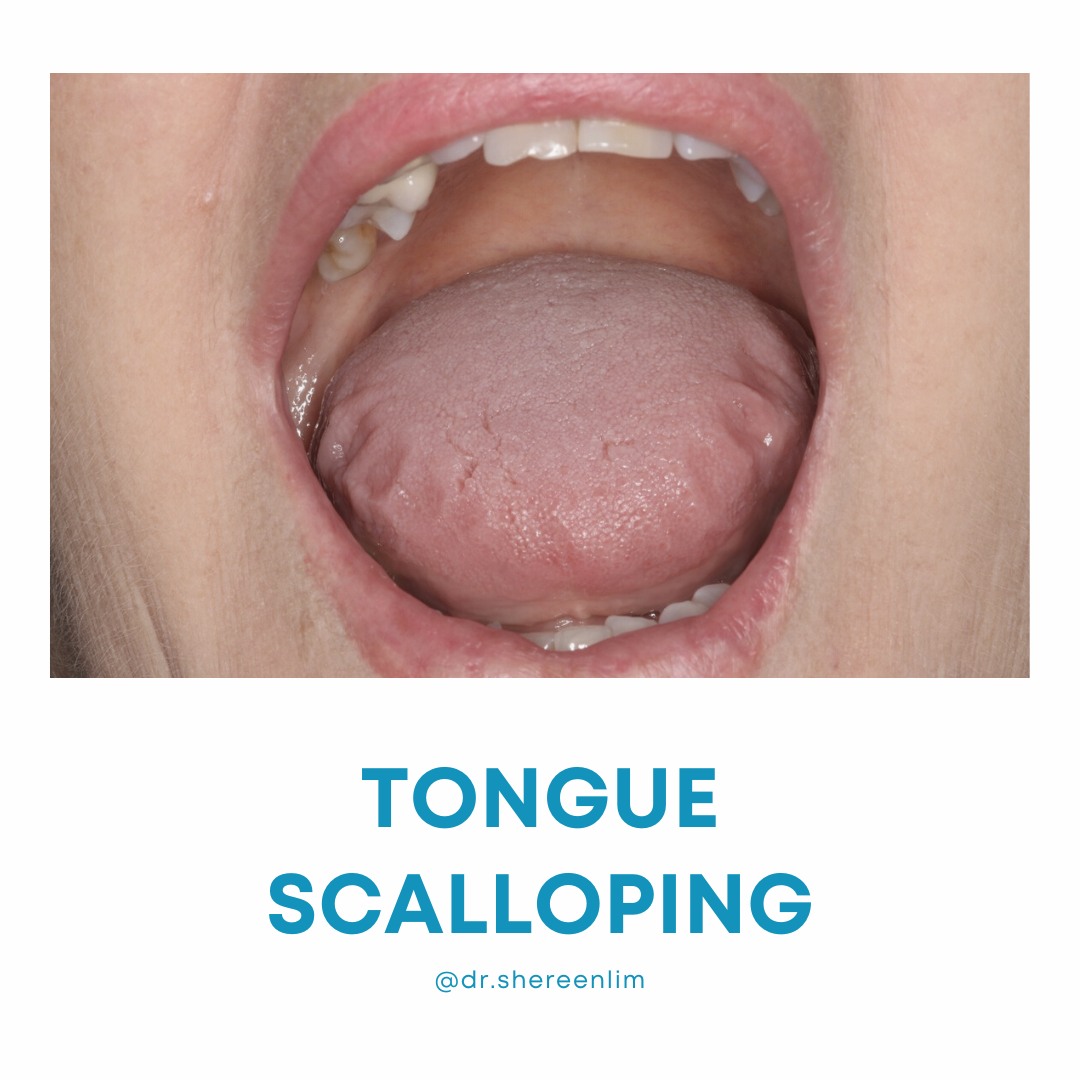
- Lowered tongue posture or tongue thrust
- Dental open bite
The problem with this pattern of facial growth is that it is linked to poor nasal passages, poor tongue space and pinched airways. This perpetuates a downward spiral of poor breathing, sleep and daytime function.
Since 60% of the face is complete by age 6 years, the best time to address mouth breathing is as early as possible. But apart from this, nasal breathing is the first line of defense against allergens, bacteria and viruses in the air we breathe. It also helps us sleep better, learn and concentrate best, and helps avoid the development of other myofunctional disorders affecting swallowing, chewing and speech.
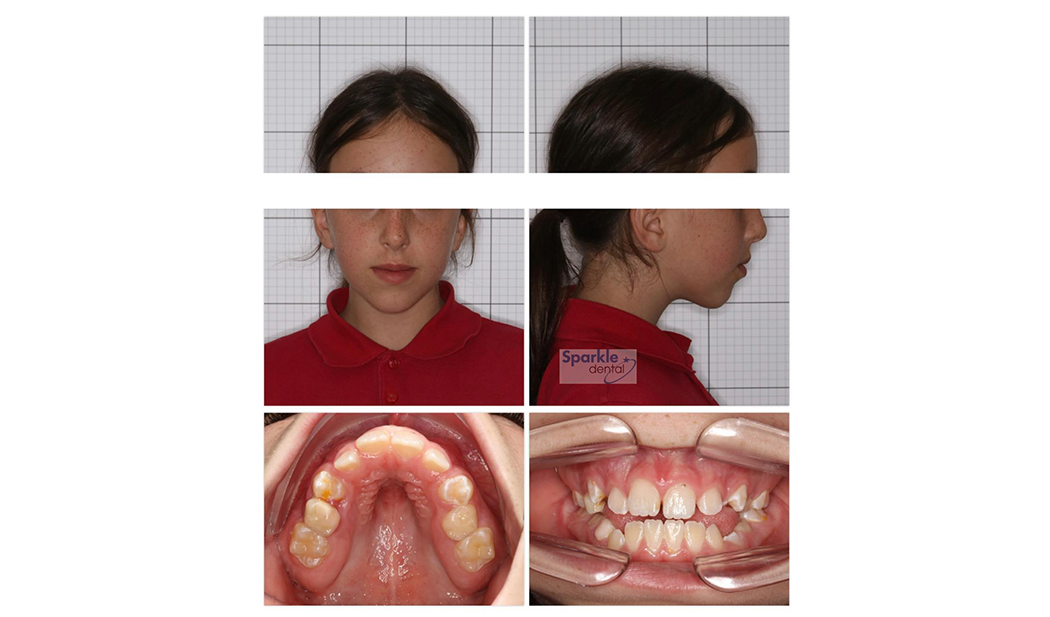
This 9.5-year-old with adenoid facies presented to me this week for a consultation regarding chronic mouth breathing. Her mum wanted to help her develop a better jaw line.
Mum described how she has always had her mouth open since birth. She has had surgery to remove her adenoids at age 2, and when they grew back, she had the surgery redone with tonsil removal at age 7 years.
Nasal obstruction and mouth breathing has persisted and there is some snoring. There are concerns with emotional regulation, facial and body tics and she suffers with regular headaches.
Occasionally she has episodes in the day where she complains she can’t get enough air, and panics. She needs to roll open the car window or be in a room with good air circulation.
When I examine her, she struggles to breathe through her nose with her lips closed.
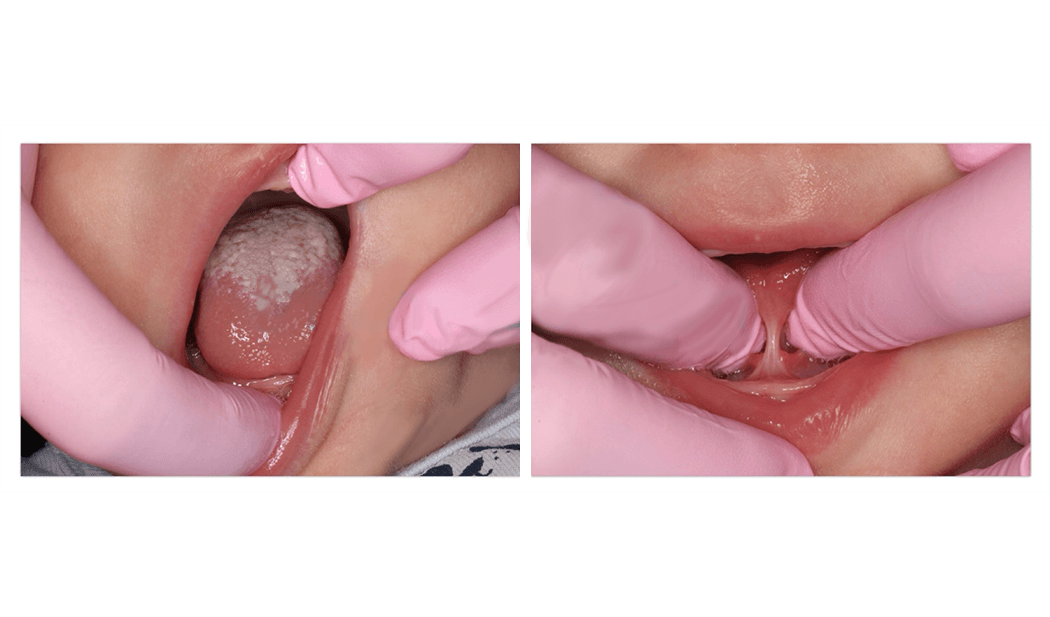
One of the standout clues of dysfunctional breathing in her mouth is the extremely narrow or gutter palate. This is linked to a severely narrow nasal floor and passage, and her tongue has no room to fit comfortably if she closes her lips.
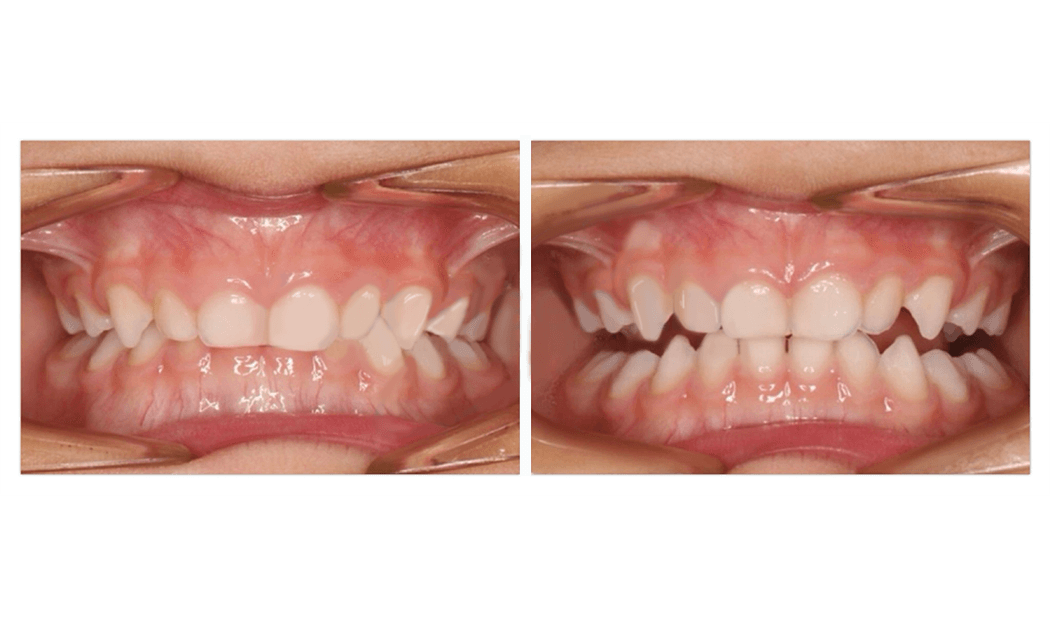
Mum explained she had recently been to the orthodontist for consultation about palate expansion, but they had said to wait until the permanent teeth come through.
The problem with waiting another 1-2 years to optimize her jaw structure is that we are missing the opportunity to promote better nasal airflow, and to see improvements in quality of life.
Furthermore, traditional expansion is less effective at improving breathing outcomes as children get older because the palate suture that needs to be opened to stimulate new bone at the nasal floor begins fusing around the age of 9 years.
Like many parents, mum wanted to know “Why didn’t anyone tell me this before?”
The answer to that is, that most of us dental, medical and allied health care professionals have received no training on this.
This is an area of increasing knowledge, and ten years ago, I would not have paid attention to the roof of the mouth and understood the significance myself.
The only reason I have developed a more holistic perspective is that I was determined to trace back the origins of breathing problems impacting sleep after seeing so many adults struggle with these issues. I committed to extensive travel, courses and workshops in fields as diverse as lactation, speech and feeding, myofunctional therapy, tongue ties, orthodontics, sleep medicine and ENT surgery to help connect more dots. I closely follow the latest research in this area, and the new evidence guides what I do in practice.
Wider change will be slow. It will take time before these new perspectives are more widely incorporated into health care and into medical and dental training.
In the meantime, this post is to help connect the dots for you as parents.
The main points to take home are:
- Restoring closed mouth breathing at the earliest age possible is ideal for facial development, sleep, behaviour and learning.
- Don’t overlook the contribution of narrow palate to breathing dysfunction
- If there is a narrow palate and breathing problems, palate expansion can be a very good option to help improve nasal airflow – it’s not just about the teeth.
- If your child has adenoid and tonsil surgery to help them breathe, it is worthwhile to book a consult for an evaluation of the palate. New thinking is that constricted palates may be a root problem contributing to the enlargement of these tissues, and that tends to fit with what Ive observed in practice.
When my team took this patient’s photos, their hearts sank to see this palate as they well recognized behind it was a story of a child falling short of their potential.
I believe in a future where this can also be recognized by every lactation consultant, paediatrician, allergist, ENT surgeon, speech and feeding specialist, dentist and orthodontist, and many more and that parents are made aware of the option of palate expansion sooner rather than later.
Look out for an upcoming post on an infant I saw yesterday headed down this same track, which will be aimed to help more people recognize the earliest warning signs.
Help spread the word by sharing this post!