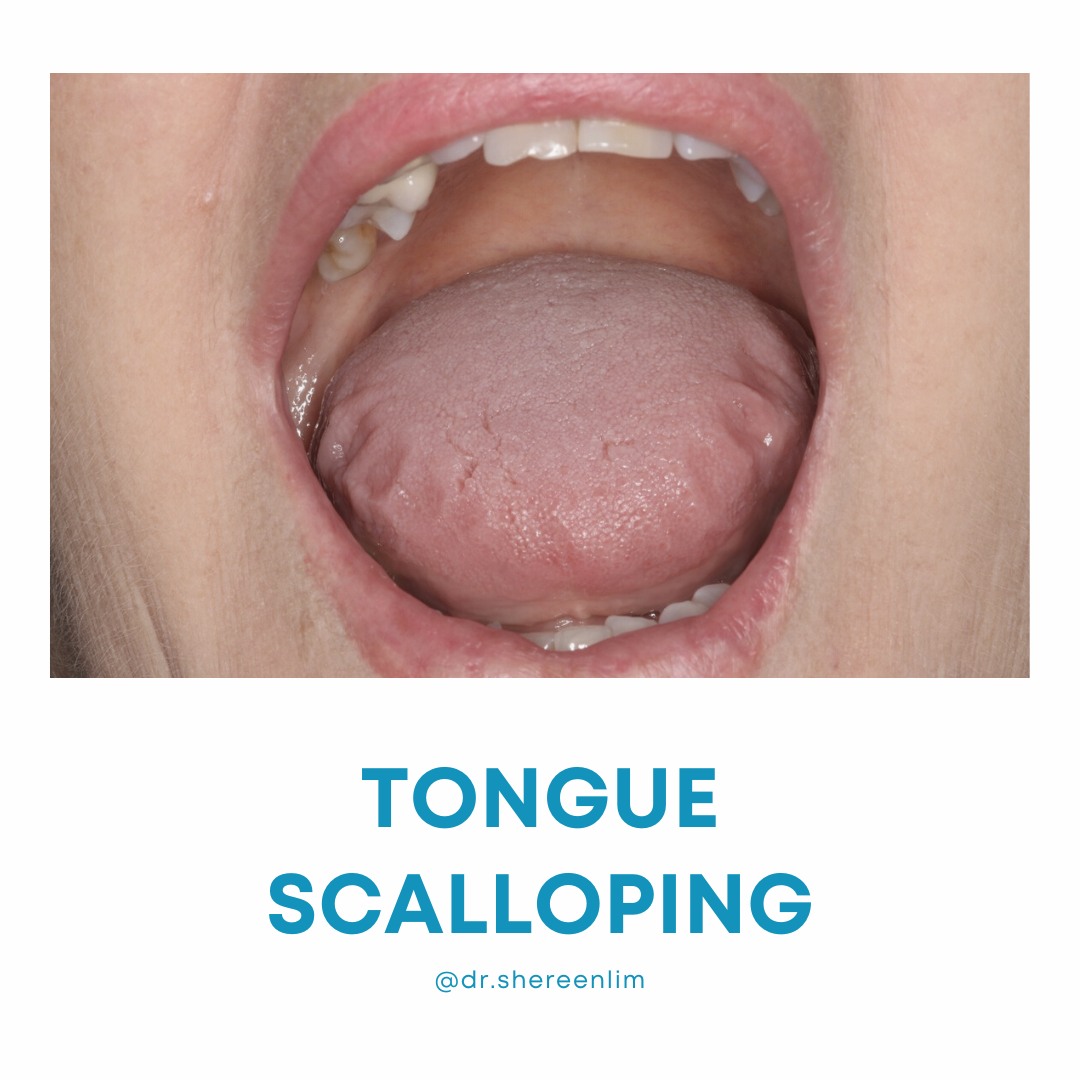
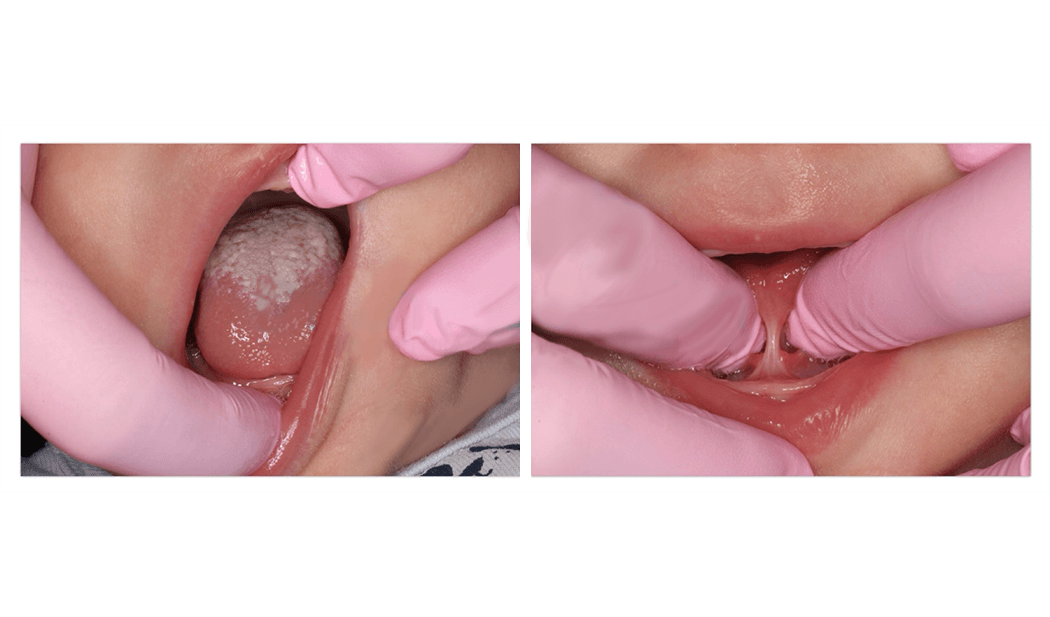
If a child is unable to elevate the tip of the tongue to their palate, without touching the teeth when asked, this can be described as tongue motor immaturity.
It could be a marker of disturbed breathing during sleep.
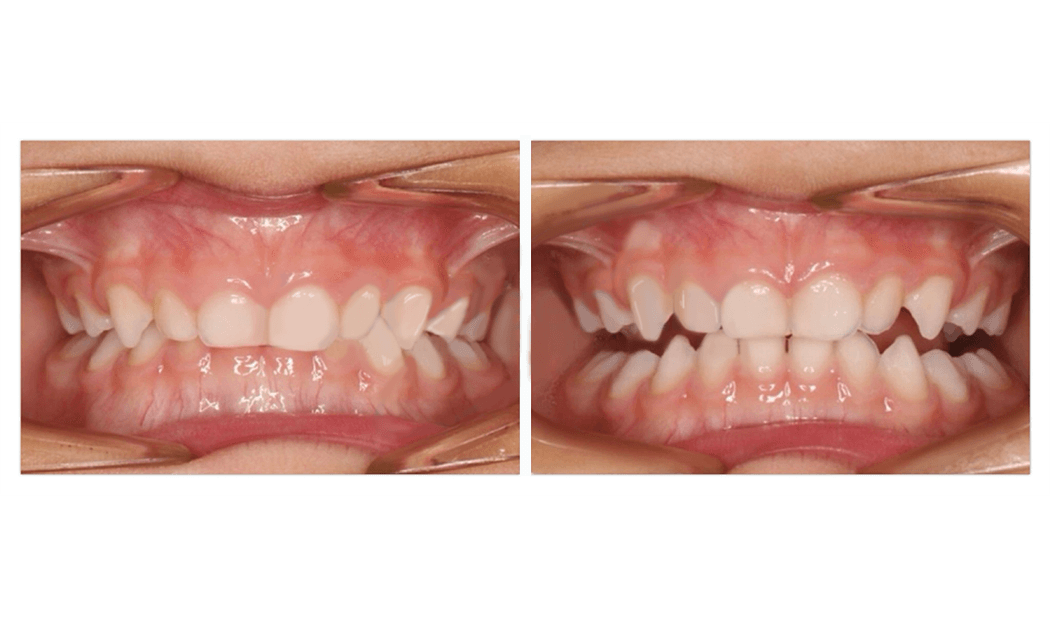
A comprehensive study analysing the jaw, dental and oral muscle characteristics of 100 children with persistent obstructive sleep apnoea after removal of adenoids and tonsils found that 24% of these children could not lift the tip of the tongue to the palate. Sleep studies demonstrated these children tended to have more severe breathing disturbances compared to those who could.
This tends to highlight that we must pay attention to how well the tongue works. This is because the bulk of the tongue is formed by the genioglossus muscle which is the main muscle responsible for keeping our throat open during sleep.
The study also found that mouth breathing was a common finding in these children, affecting 62% of children.
More common than nasal abnormalities like cartilage hyptonia (18%), deviated nasal septums (5%) or nasal obstruction (32%), was the contribution of tongue tie/restricted tongue mobility (40%) and narrow palate (42%). These factors contributed to low tongue posture and could be a factor in the lack of tongue to palate seal and persistent of mouth breathing.
In practice, I have observed this lack of tongue coordination/tone is often also linked to issues including poor speech articulation, difficulties chewing and swallowing meat, or glue ear, and even difficulties hearing in this child’s case.
If you want to read more about the study, here is the link.
Prevalence of malocclusions and oral dysfunctions in children with persistent sleep-disordered breathing after adenotonsillectomy in the long term
https://jcsm.aasm.org/doi/pdf/10.5664/jcsm.8534