Yesterday I saw eight expansion patients between the ages of 3-4 years. It made me reflect on how much younger my patient base is becoming, how impactful I’m finding it, and my journey starting treatment younger and younger.
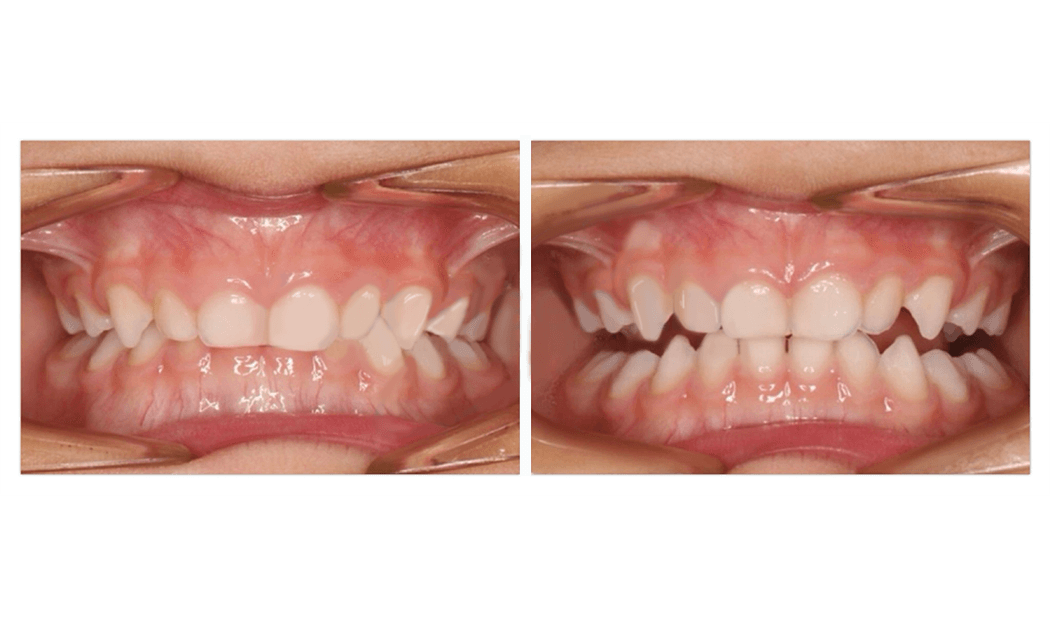
The traditional age for expansion is age 7-8 years when the first permanent teeth start to come through.
But five years ago, I made a brave decision that I was going to expand my youngest daughter’s palate at age 6.
This was especially because that was before the days of digital scanning at Sparkle and I had to subject her to bulky and messy impression materials that was never a fun experience for any child!
She had persistent symptoms of disturbed breathing during sleep after earlier surgical removal of adenoids, tonsils and turbinate reduction. Symptoms included teeth grinding, very wet pull ups at night, and she was the type of child you wouldn’t want to go to bed with, doing 360 turns all night long in bed. Her teeth were wearing away, and she was starting to feel self conscious when we bought pull ups at the shops. I was running out of options to address the underlying airway problem and if palate expansion was helping 7 year olds, why wouldn’t it help her?
Her symptoms resolved within a month of treatment, her sleep was sounder, and the bonus was it made more space for her first permanent teeth to come through in good alignment. Age 6 became my new ideal age to start treatment and I thought I was doing a great service.
Two years ago, influential colleagues in the US challenged me further to start even earlier.
There’s always the professional concern that treatment can be more efficient and less costly for patients if we can delay the start of treatment.
However my colleagues gave the analogy that delaying treatment is like telling parents not to get glasses for their child until age 8 when a vision problem is detected much earlier. Yes, it rules out them needing a new pair as they grow bigger. But what experience will they miss waiting and watching for those extra years?
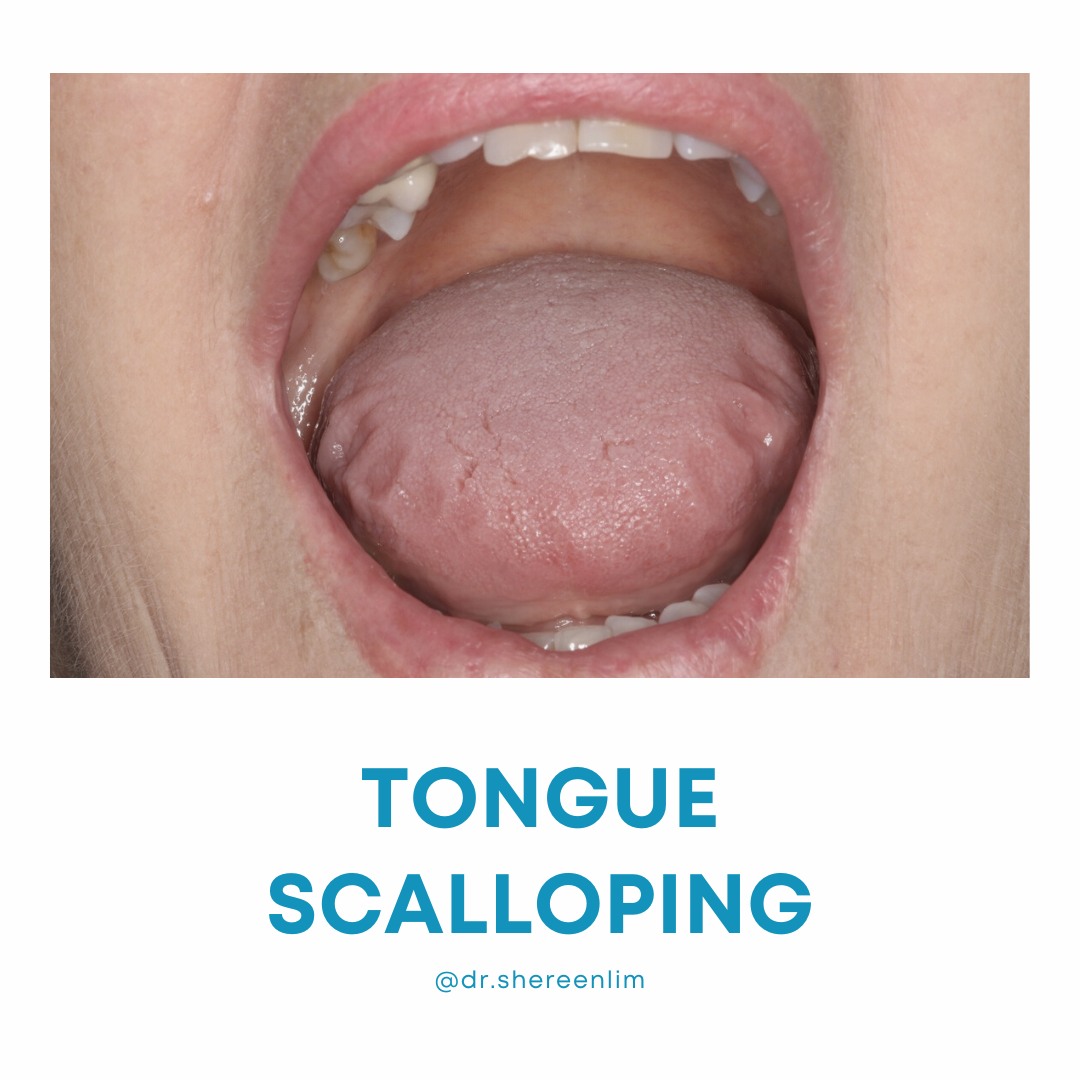
You see the palate is the floor of the nose and the housing for the tongue. The narrow palate is a known risk factor for obstructive breathing during sleep. But when growth is off track to any degree, there is some degree of airflow limitation and breathing and sleep will not be the best it could be.
Two important studies that followed 11,000 children found mouth breathing, snoring and gasping during sleep in the earliest years of life increase a child’s risk of behavioural and socio-emotional problems, and special education needs at age 4 and 7, even when the breathing problems have peaked and subsided at age 30 months. We can’t predict exactly which children will be most affected. But I’ve seen enough of the 7-8 year olds who are on wait list to see a paediatrician for an ADHD diagnosis or who are already being medicated, to question the watch, wait and roll a dice approach.
That’s why I think it’s important our profession offers parents the info and choice to start treatment earlier than we have in the past.
Honestly, we used to be a practice where none of the dentists were eager and comfortable working with young children, and our front office team used to cringe when parents had a great experience and wanted to bring their children too.
But now, thanks to the support of our talented with children team, I really enjoy our little patients, and am rewarded knowing we are helping them achieve a better trajectory of development.
I’m not promising we can manage ADHD.
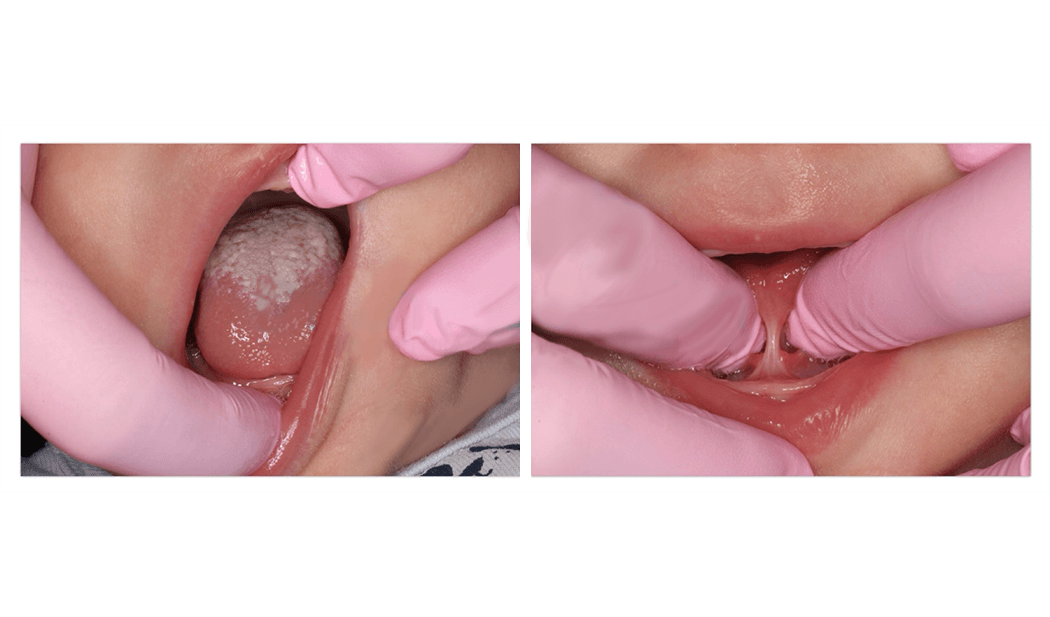
But I do think we need to focus on health and not letting symptoms compound, and that includes optimising jaw and airway development, breathing and sleep. This photo is a throwback to my first 3.5 year old patient that I had the privilege of treating! How could I not love this work with patients as adorable as her!